Baqara2/2: This is the book in which there is no doubt (about it being the word of God), it is a guide for Muttaqin
Ale-Emran138/3: This (reality that systems govern human society, not faith or chance occurrences) is a clear exposition for all people, and a guidance and admonition for the God-conscious (Muttaqin)
THE STRAIGHT PATH: CONTEMPORARY INSIGHTS FROM THE QURAN
Copyright © 2024 Mohammad Farivar,
ght © 2024 Mohammad Farivar, All Rights Reserved
International Rights Secured
No part of this book may be reproduced or used in any manner without written permission of the copyright owner except for the use of quotations in a book review.
ISBN: 979-8338352045
The author appreciates Mr.Morteza Parizi of Pars Publishing and Dr. AR Haghighi for their significant contribution towards preliminary English translation and editing
Disclaimer
Table of Contents
Disclaimer........................................................................................2
Preface of English Translation.........................................................I
Preface - First Edition ................................................................... IV
Preface - Second Edition..............................................................XV
Keywords in the Quran .............................................................XVII
Chapter 1: The Quran is the word of God and revelations to the
Prophet (pbuh) .................................................................................1
Recitation, Chanting, and Thinking in the Quran (Tilawah,
Tajwid, Tadabbur)....................................................................... 6
Religion/Din:............................................................................. 11
Islam and Muslims.................................................................... 16
Tasbih/Subhan Allah (Praise be to God, performing assigned
corrective action) ...................................................................... 19
Salat/Prayer/Namaz: ................................................................. 22
Chapter 2: The Quran and Human Creation .................................26
Chapter 3: Human Nature (Fitrah) According to the Quran.........41
Carnality and Primitive Soul (Nafs Al-Ammara)..................... 43
Upbraiding Soul (Moral)........................................................... 44
Confident Soul (Spiritual)......................................................... 45
Human Nature (Temperament)................................................. 48
Temperament and States of the Ego ......................................... 49
Carnality, Natural, Primitive, Lustful (Nafs Ammarah)........... 50
Upbraiding Soul, Reproving Soul, Moral (Nafs Lawwamah).. 50
Tranquil Soul and Spiritual (Nafs Mutma'innah) ..................... 51
Chapter 4: Ebadat..........................................................................54
What is the meaning of Abdollah (God’s slave)?..................... 59
Man as the Caliph of God ......................................................... 62
Worship/Ebadat (serving God through righteous deeds).......... 67
Observance of Moderation in Worship:.................................... 69
Sacrifice, Struggle, and Jihad.................................................... 73
Chapter 5: Dua (Request from God, Devotion, prayer, supplication)
........................................................................................................75
The Quranic supplication (Dua) as a Model to be emulated .... 85
Briefly divine prophets and possessors of wisdom and insight ask
God for:..................................................................................... 85
Quranic supplication verses in order of Surahs: ....................... 86
Chapter 6: Salat.............................................................................99
Salat times:.............................................................................. 102
Salat framework:..................................................................... 106
The seven verses of Surah Al-Fatiha: ..................................... 112
Master of the Day of Judgment............................................... 115
We worship and serve You only............................................. 116
Guide us in the straight path. .................................................. 117
According to Surah Hamd, people are divided into three groups
by God:.................................................................................... 120
Qunut: ..................................................................................... 122
Tashahhod (Testifying):.......................................................... 122
Sura Naas (mankind) 114........................................................ 141
Surah al-Falaq 113, or The Dawn:.......................................... 142
Surah Ma'oun 107:.................................................................. 143
Chapter 7: Explanation and description of the straight path.......144
God has made mercy obligatory upon Himself. ..................... 153
Ten Commandments in the Qur'an to improve individual life.
................................................................................................. 154
Ten Commandments from the Qur'an to reform society: ....... 155
The History of Straight Path ................................................... 157
Commandments of Prophet Noah: .......................................... 158
The Ten Commandments of Prophet Moses ........................... 159
Straight path in the Bible: ....................................................... 160
Straight path and Buddhism: ................................................... 162
Enlightenment and the Straight Path ....................................... 167
Traits of the truthful (Seddiqin): ............................................. 195
Verses related to going astray (lost, Zal’lin). .......................... 203
Chapter 8: Fasting .......................................................................205
The Night of Qadr
Goodly loan (Hassana) ............................................................ 225
Usury (Riba)............................................................................ 226
Chapter 10: Enjoining good and preventing evil. .......................228
Chapter 11: Moral virtues and vices ............................................242
A history of morality ............................................................... 242
Satan's temptation ................................................................... 250
Jealousy, Pride, and Arrogance
........................................................ 253
............................................... 251
Sins: Moral and Religious
Different Sins have different consequences: ................. 255
................................................................... 208
Features of the pious (muttaqin) who are guided by the Quran..209
Chapter 9: Zakat, charity, Donation, interest-free loan ..............214
Charity/Almsgiving (sadaqa) and Donation (infaq) ............... 216
Abraham was a Hanif; what does Hanif means? .................... 222
Sherk (polytheism): ................................................................. 260
Fesq (debauchery): .................................................................. 265
Sins with worldly punishment: ............................................... 266
Theft: ....................................................................................... 267
Adultery (sexual relation with a married woman): ................. 270
Qisas (revenge, retribution punishment of homicide in justice):
................................................................................................. 275
Extravagance and balance: ...................................................... 277
Alcohol consumption and gambling: ...................................... 277
Halal and Haraam (forbidden) foods ...................................... 282
Oppression (Zolm): ................................................................. 283
Forgiveness of sins:................................................................. 285
Chapter 12: European Enlightenment Era ..................................296
From Birth to Seventeen Years Old ........................................ 298
Nain now revels in the fruits of Western Enlightenment. ....... 304
USA and its Democratic Constitution..................................... 311
Roxbury Latin High School, an Exemplary Educational System
................................................................................................. 322
Jews and the reasons for their success (successful Ummah) .. 328
The reasons for the success of the Jews: ................................. 333
Chapter 13: Updating Jurisprudence ...........................................338
Verses about Prophet Mohammad (PBUH) in Quran..... 342
Does the present time requires a review of Islamic law and
jurisprudence? ......................................................................... 346
1. Hanafi:................................................................................. 348
2. Maaleki: .............................................................................. 349
3. Shafe'i .................................................................................. 349
4. Hanbali: ............................................................................... 350
5. Salafi and Takfiri (Wahhabis, Divbandi, and Muslim
Brotherhood):.......................................................................... 350
Shiite religions:....................................................................... 351
The difference between Shia 12 Imami and Sunni schools:... 352
Abrogated and annulled Quranic decrees during prophet life
(aayate Nasekh va Mansukh).................................................. 355
AQL (reasoning)..................................................................... 366
What should be done for Islam today? What is moral and straight
path today? .............................................................................. 369
Chapter 14: Conclusions.............................................................382
References....................................................................................415
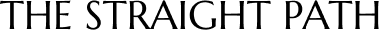
Preface of English Translation
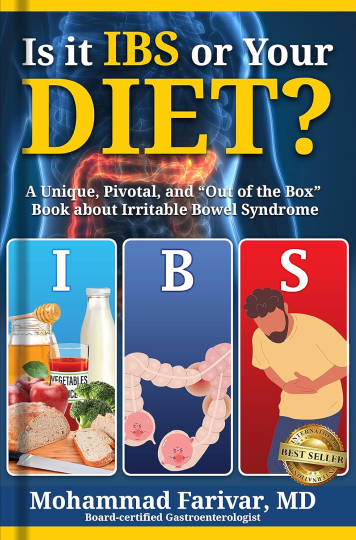
In this English translation of the book "Straight Path according to the Holy Quran," I have retained the preface to the first edition in Farsi, in case the reader wishes to become more familiar with my background and motive in writing this book.
This special introduction to the English translation aims to briefly outline the topics discussed based on the Quran and invite readers to contemplate what real Islam entails and what a true Muslim should be.
The problem for Muslims has been that for important duties towards God, we have taken the easy way out by merely performing them rather than embodying their essence. Examples like Salat, Tasbih, and Dua have been reduced to mere rituals termed "Ebadaat." We have misunderstood the Quranic meanings of Din, Islam, and Muslim. We often claim to be Musalmaan based on our place or family of birth.
When performing Salat, we ask God 10 times daily to guide us on the straight path, but what does this straight path entail? No book has been written about the straight path as far as I am aware. When asked what the straight path is, the common answer is "doing the right thing," rather than understanding what God recommends in the Holy Quran and expects us to do through His message in our daily Salats.
The Quranic meanings of various subjects like Din, Islam, Muslim, Tasbih, Dua, Salat, and the Straight Path is often misunderstood by Muslims, leading to our collective astray and social retardation. This book delves into these subjects to shed light on their true essence and significance.
- **Din**: Encompasses following the laws enacted by God, which are universal and the same for all human beings. Judaism, Christianity, and Islam are different branches of the same basic Din, with varying commands according to time, place, and culture.
- **Islam**: Involves submission to and acceptance of God's constitutional laws.
- **Muslim**: Refers to one who accepts and practices the recommended laws
- **Tasbih**: Should entail actively participating in the duties assigned by God, rather than mere verbal repetitions.
**Dua**: Should involve asking God to help reach life goals over time through hard work, with a lofty purpose. In that case, the laws of the universe will be at your service and will facilitate reaching your target goal.
- **Salat**: Means getting in touch and connecting with God, seeking guidance in the straight path in all aspects of life.
- **Straight Path**: Refers to staying in the middle and choosing the shortest way to be useful and happy, as recommended by various prophets including Moses,
Jesus, Buddha, and Mohammad.
- **Enjoining Good and Prevention of Vice**: Involves personal and familial responsibilities, with an emphasis on education and law-abiding behavior. Citizens have the duty of guiding government officials to do well and prevent harm to their citizens, not the other way around.
- **Jihad**: In the Quran, is defensive and not offensive, with the major Jihad being against one's own ego and self-restraint.
- **Ebadaat**: Muslims have misconceived daily prayers, fasting, and other rituals as mere exercises, neglecting their true purpose of embodying God-like qualities and working to make the world a better place.
This book advocates a return to the Quran, reason, and learning from successful democratic societies. It discusses the need for reform in Islamic jurisprudence, particularly concerning women's rights and personal-social-political aspects of Sharia. The text also highlights the achievements of non-Muslim societies in various fields, urging Muslims to engage more with modern advancements and become active participants in global civilization.
In essence, " Sirat al-Mustaqim" is a call-to-action for Muslims and non-Muslims alike to cultivate a world of harmony, respect, and enlightenment, aligning with the spirit of the Quran and the needs of modern society. It emphasizes universal Islamic values of knowledge, honesty, and compassion, urging readers to embrace lives of purpose and integrity.
Preface - First Edition
My grandson Cyrus, who was born in America, asked me when he was 13 years old about the meaning of "Show us the Straight Path" in the daily obligatory prayers (Salat). I gave him an answer that I thought was convincing, but it was clear from his expression that he was not satisfied with my general explanation and was looking for a more comprehensive answer. I promised him that during my upcoming trip to Iran, I would bring him a book written in English about the straight path. Unfortunately, after visiting many bookstores and asking reputable booksellers and authorities, I found that no such book had ever been written in Farsi, Arabic, or English.
I decided to keep my promise and personally research this issue to provide him with an acceptable response based on the Holy Quran. Using numerous reliable sources, several conflicting questions related to the straight path were brought to my attention, which took a long time to address. I decided to use only the Holy Quran as a reference. In writing this book, I thought that in addition to Cyrus, who is a third-generation immigrant in America, it would be useful for the second generation, many first-generation immigrants, and non-Muslims who are not familiar with the Holy Quran and want to know more about it.
My background, with very limited knowledge of the Quran, practicing medicine in the USA, and various trips to Muslim and non-Muslim countries for charitable and public benefit activities, particularly in Iran, the Middle
East, and the USA, has taught me that there are different meanings in some religious concepts and different ways of life, which will be explained later.
I was born in the small city of Nain in the Isfahan province of Iran in 1945 and lived there until I finished high school. The lifestyle in Nain had did not seem to have changed significantly over the past thousand years, I believed. The next seven years, I went to university in Tehran, which was a completely different environment compared to my hometown. In my fifth year of medicine, I met and married my wife, who was from Kashan and a student of Social Sciences. In 1970, I obtained a doctorate in medicine, and in 1971, about 8 years before the Islamic Revolution, I immigrated to the USA with my wife and two-year-old son Saeed for post-doctoral education.
My knowledge of the Arabic language and the Quran was at the high school level at that time, limited to Salat prayer, fasting, principles and branches of religion, Surah Hamd, Chahar Qol, Ayat al-Kursi, the story of Imam Hussain, the incident of Karbala, the Muharram and Ashura ceremonies, and the fervent prayers in the nights of the revival of the holy month of Ramadan. My daily obligatory prayers and fasting were few and far in between. I was the first person in my family with a high school diploma, and the only religious book I had read was a very limited text about the principles of Islam that we studied in high school at that time, and the prayer recitations of the Muharram nights in the neighborhood Husseinieh. The most important lessons about Islam were listening to several sermons of the late Grand Ayatollah
Seyyed Javad Gharavi Isfahani (may God bless his soul and grant him peace in the Hereafter) who gave sermons for the public in the afternoon of the holy month of Ramadan for a couple of years in the bazar’s Khaja Mosque.
Continuing education in the USA, being too busy to take care of the affairs of a young family of five and an immigrant, getting to know and adapting to a new culture and environment in every way, a responsible career in successful medicine with academic appointments at the medical schools of Boston University and Harvard University, and responsibilities as head of the department and board member in different hospitals, had consumed me in my VI profession, so I didn’t even think about thinking let alone researching about Islamic topics due to the lack of need.
For historical and cultural reasons, Boston is one of the oldest cities in the USA and the closest to the definition of utopia and a "city on the Hill with a guiding light". In Boston, people are often literate, knowledgeable, philanthropic, honest, and respect the rule of law. Harvard and MIT universities and dozens of prestigious universities and colleges are located here, and there are quite a few Nobel Prize winners in different fields who live here. Years of active professional and social life there have made me attuned to the morals and way of thinking of Bostonians.
In the early years after the revolution and a couple of years before that, a group of Iranians left their country willingly and/or unwillingly, and a few chose Boston as their second home for career, cultural, and educational reasons. This group was mostly educated in the USA, and they have been the source of important governmental and non-governmental works in Iran before the revolution. There was also a group of capitalists who had migrated there after the self-exile due to the presence of world-renowned universities in Boston and the future of their children.
For several reasons, such as living in the USA for several years, fame and practice of medicine, various guidance needed by newcomers, etc., in the gatherings I was often invited too, I frequently observed that most families gradually distanced themselves from their imported Islam. For example, wearing a headscarf/Hijab would go away, the skirts would get shorter and above the knees, some women would have cigarettes in their hands and the men would have different and expensive alcoholic drinks. In other words, they were absorbed in their unique environment, and their Islam was summed up in the presence of a volume of the Quran at home. In frequent friendly gatherings at night, the discussion and entertainment often revolved around Iranian politics, Islam, the VII religious government, and the mullahs’ Velayat Faghih system. They often mixed true Islam with the Islamic government of Iran and trampled religion and government with their own foul language. Sometimes, contrary to their expectations, they heard words in
support of religion from me, which was based on my honesty and previous information, telling them that true Islam should be separated from the religion represented by the government and their politics because the two are not synonymous.
One day, one of these newly arrived friends, who was old, literate, honest, famous, a source of service, belonging to a very famous religious and cultural family, knowledgeable, and, according to his own words, benevolent and well off, gave me a book called “23 years”, which they said was written by Senator Ali Dashti. It was a photocopy being passed from hand to hand among the elder people. He lent it to me to study and clarify my thoughts. In this book, the author has described the life of Mohammad during the 23 years that he lived after prophethood with a biased understanding of a small portion of the Quranic verses, which were discussed and ridiculed. It was clear that its only purpose was the reader’s apostasy from Islam. Reading this book would easily satisfy the desired effect of the author. I thought about its contents day and night.